CLINIC DR.PRINYA HATYAI SONGKLA THAILAND
LASER SKIN PROCEDURES and COSMETIC SURGERY


Hemorrhoids (Piles)
Treatment cost
Sclerosing injection 1,000 Baht/head
Rubber band ligation 500 Baht/head
Surgery 5,000 Baht/head
Laser Surgery 8,000 Baht/head
What Are Hemorrhoids?
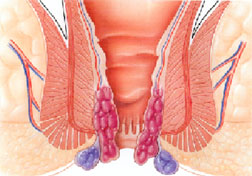
The term hemorrhoids refers to a condition in which the veins around the anus or lower rectum are swollen and inflamed. Hemorrhoids may result from straining to move stool. Other contributing factors include pregnancy, aging, chronic constipation or diarrhea, and anal intercourse. Hemorrhoids are both inside and above the anus (internal) or under the skin around the anus (external). Hemorrhoids (piles) arise from congestion of internal and/or external venous plexuses around the anal canal.
Hemorrhoids are classified into four degrees, depending on severity, so that they can more easily be evaluated for possible surgery. For more detailed information, view our page Surgical Classification of Hemorrhoids.
What Are the Symptoms of Hemorrhoids?
Many anorectal problems, including fissures, fistulae, abscesses, or irritation and itching (pruritus ani), have similar symptoms and are incorrectly referred to as hemorrhoids. Hemorrhoids usually are not dangerous or life threatening. Rarely, a patient can have bleeding so severe, that severe anemia or death may occur. In some cases, hemorrhoidal symptoms simply go away within a few days. But in most cases, hemorrhoidal symptoms eventually return, often worse than they were before. Although many people have hemorrhoids, not all experience symptoms. The most common symptom of internal hemorrhoids is bright red blood covering the stool, on toilet paper, or in the toilet bowl. However, an internal hemorrhoid may protrude through the anus outside the body, becoming irritated and painful. This is known as a protruding hemorrhoid. Symptoms of external hemorrhoids may include painful swelling or a hard lump around the anus that results when a blood clot forms. This condition is known as a thrombosed external hemorrhoid. In addition, excessive straining, rubbing, or cleaning around the anus may cause irritation with bleeding and/or itching, which may produce a vicious cycle of symptoms. Draining mucus may also cause itching.
What is the Treatment?
Medical treatment of hemorrhoids is aimed initially at relieving symptoms. Measures to reduce symptoms include ? Warm tub baths several times a day in plain, warm water for about 10 minutes. ? Application of a hemorrhoidal cream or suppository to the affected area for a limited time. Preventing of the recurrence of hemorrhoids will require relieving the pressure and straining of constipation. Doctors will often recommend increasing fiber and fluids in the diet. Eating the right amount of fiber and drinking six to eight glasses of fluid (not alcohol) result in softer, bulkier stools. A softer stool makes emptying the bowels easier and lessens the pressure on hemorrhoids caused by straining. Eliminating straining also helps prevent the hemorrhoids from protruding. Good sources of fiber are fruits, vegetables, and whole grains. In addition, doctors may suggest a bulk stool softener or a fiber supplement such as psyllium or methylcellulose. In some cases, hemorrhoids must be treated endoscopically or surgically. These methods are used to shrink and destroy the hemorrhoidal tissue. The doctor will perform the procedure during an office or hospital visit. A number of methods may be used to remove or reduce the size of hemorrhoids, such as painless non-surgical techniques, lasers for hemorrhoids, harmonic scalpel for hemorrhoids, and the use of hemorrhoid medications.
How Are Hemorrhoids Prevented?
The best way to prevent hemorrhoids is to keep stools soft so they pass easily, thus decreasing pressure, and to empty bowels without undue straining as soon as possible after the urge occurs. Exercise, including walking, and eating a high fiber diet, help reduce constipation and straining by producing stools that are softer and easier to pass.
Surgical Treatment
Traditional Surgery
In many cases hemorrhoidal disease can be treated by dietary modifications, topical medications and soaking in warm water, which temporarily reduce symptoms of pain and swelling. Additionally, painless non-surgical methods of treatment are available to most of our patients as a viable alternative to a permanent hemorrhoid cure.
In a certain percentage of cases, however, surgical procedures are necessary to provide satisfactory, long?term relief. In cases involving a greater degree of prolapse, a variety of operative techniques are employed to address the problem.
Milligan-Morgan Technique
Developed in the United Kingdom by Drs. Milligan and Morgan, in 1937. The three major hemorrhoidal vessels are excised. In order to avoid stenosis, three pear-shaped incisions are left open, separated by bridges of skin and mucosa. This technique is the most popular method, and is considered the gold standard by which most other surgical hemorrhoidectomy techniques are compared.
Ferguson Technique
Developed in the United States by Dr. Ferguson, in 1952. This is a modification of the Milligan-Morgan technique (above), whereby the incisions are totally or partially closed with absorbable running suture.
Conventional haemorrhoidectomy can be performed as a day-case procedure.
Laser Surgery for Hemorrhoids
Skilled surgeons use laser light with pinpoint accuracy. The unwanted hemorrhoid is simply vaporized or excised. The infinitely small laser beam allows for unequaled precision and accuracy, and usually rapid, unimpaired healing.
The result is less discomfort, less medication, and faster healing. A hospital stay is generally not required. The laser is inherently therapeutic, sealing off nerves and tiny blood vessels with an invisible light. By sealing superficial nerve endings patients have a minimum of postoperative discomfort. With the closing of tiny blood vessels, your proctologist is able to operate in a controlled and bloodless environment.
Procedures can often be completed more quickly and with less difficulty for both patient and physician. Laser can be use alone or in combination with other modalities. A study of 750 patients undergoing laser treatment for hemorrhoids reported successful results of 98%. The patient satisfaction was 99%.